Objective: The aim of this study was to determine if male sex is a poor prognostic factor for developmental dysplasia of the hip (DDH) and to determine the mid-long-term radiological and clinical results of male patients in comparison with female patients following an open reduction with posteromedial limited approach.
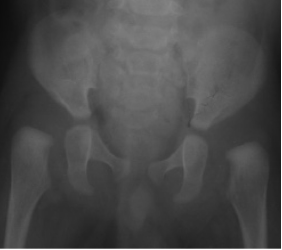
Methods: We examined 54 hips of 41 male patients (12.38 ± 4.82 months) and 96 hips of 82 female patients (11.11 ± 4.93 months) with DDH. All the patients underwent open reduction with posteromedial limited approach. The average follow-up time was 108 months for the male patients and 110 months for the female patients. The Tonnis grade, acetabular index, Kalamchi and MacEwen classi € fication, and Severin classifications were determined for all patients. The Mc Kay classification system was used to evaluate the functional results.
Results: From the total, 25 (60%) male and 70 (85%) female patients had satisfactory radiographic outcomes (Severin Ia, Ib, or II) according to the Severin classification. There was a significant difference between the two groups in terms of the Severin classification (P ¼ 0.04). Residual acetabular dysplasia (RAD) was observed in 12 (15%) female and 17 (41%) male patients (P ¼ 0.001). Grade 2 or higher osteonecrosis was observed in 7 (9%) patients in female and 6 (15%) patients in male group. The clinical outcomes in terms of the Mc Kay classification showed satisfactory outcomes in 72 (87%) female and 34 (82%) male patients. Further, 8 (9.7%) female patients and 6 (14.6%) male patients underwent a second operation. However, there was no difference between the two groups in terms of postoperative osteonecrosis presence (P ¼ 0.982), functional outcomes (P ¼ 0.571), and secondary operation rates (P ¼ 0.298). Male sex was associated with poor outcomes in terms of the Severin classification (P ¼ 0.04) and RAD (P ¼ 0.001).
Conclusion: Although our results indicated that male sex is a poor prognostic factor for radiological results and RAD, there was no difference between male and female patients in terms of osteonecrosis, redislocations, and functional outcomes. Secondary surgical interventions should not be delayed in the absence of the spontaneous development of acetabulum.
Level of evidence: Level III, prognostic study.


.png)
.png)